RCM Performance Suite
Elevate revenue cycle results with precision intelligence and full audit traceability.
Challenges
Revenue cycle workflows break when high-complexity diagnostics (e.g., genomic sequencing) face rigid payer policies. Generic billing tools cannot handle the nuance of molecular coding, leading to massive revenue leakage.
Prior Authorization Bottlenecks
Complex tests require detailed clinical evidence. Manual submission is slow and missing "medical necessity" documentation leads to automatic rejections and written-off tests.
High Denial Rates
Payers frequently flag molecular CPT codes as "experimental" or "not medically necessary." Appeals require expert clinical arguments that standard billing teams cannot generate at scale.
Patient Financial Surprise
Patients are often unaware of high out-of-pocket costs for specialty tests. The lack of upfront transparency leads to bad debt and high abandonment rates.
Coding Complexity
Mismatches between genetic results and ICD-10 codes trigger immediate claim rejections. Keeping up with constantly changing payer-specific coding rules is manually impossible.
What Defines Us
Transforming lab and device billing with clinical intelligence that bridges the gap between scientific results and reimbursement policy.
Intelligence tailored for revenue integrity and operational clarity.
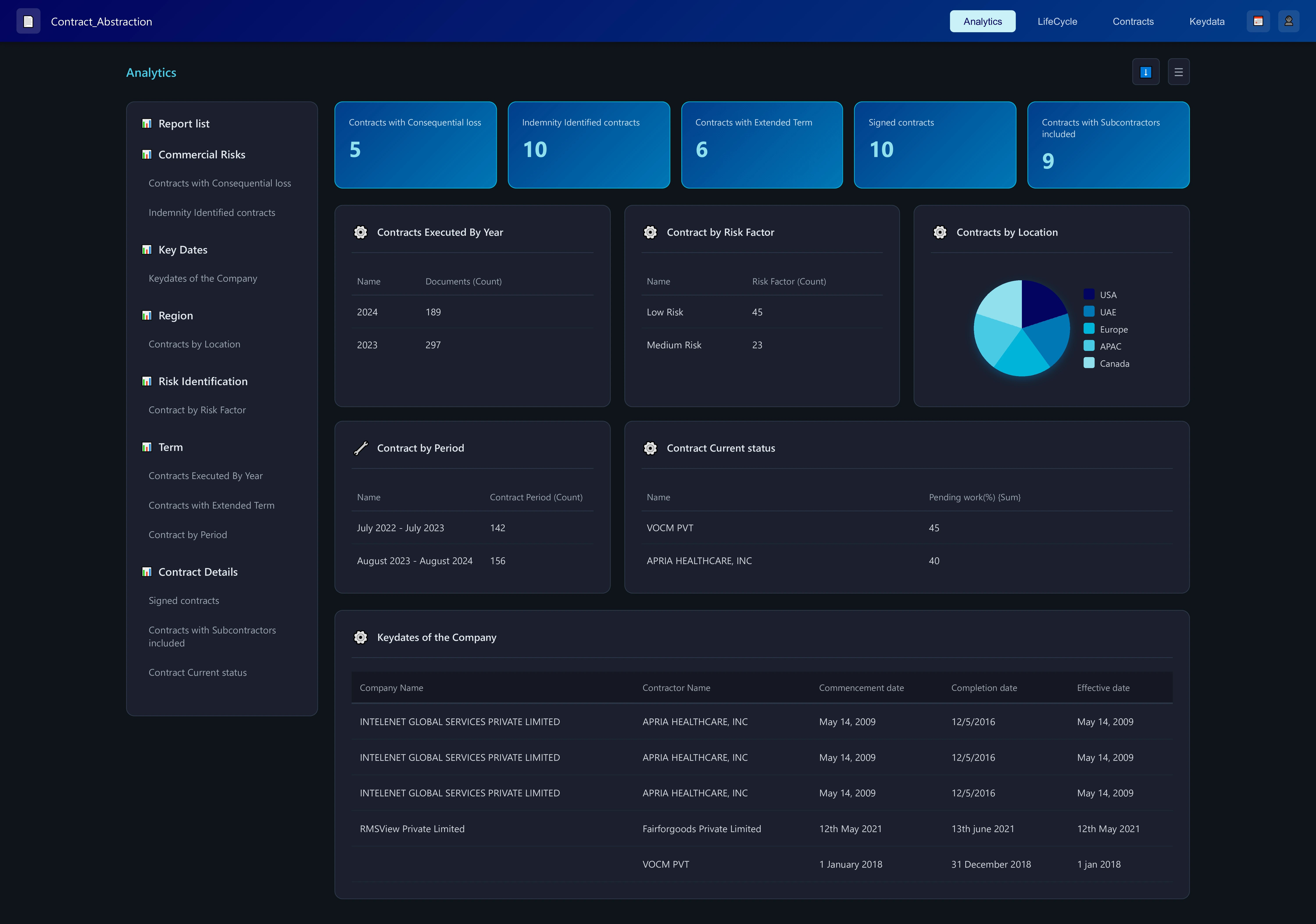
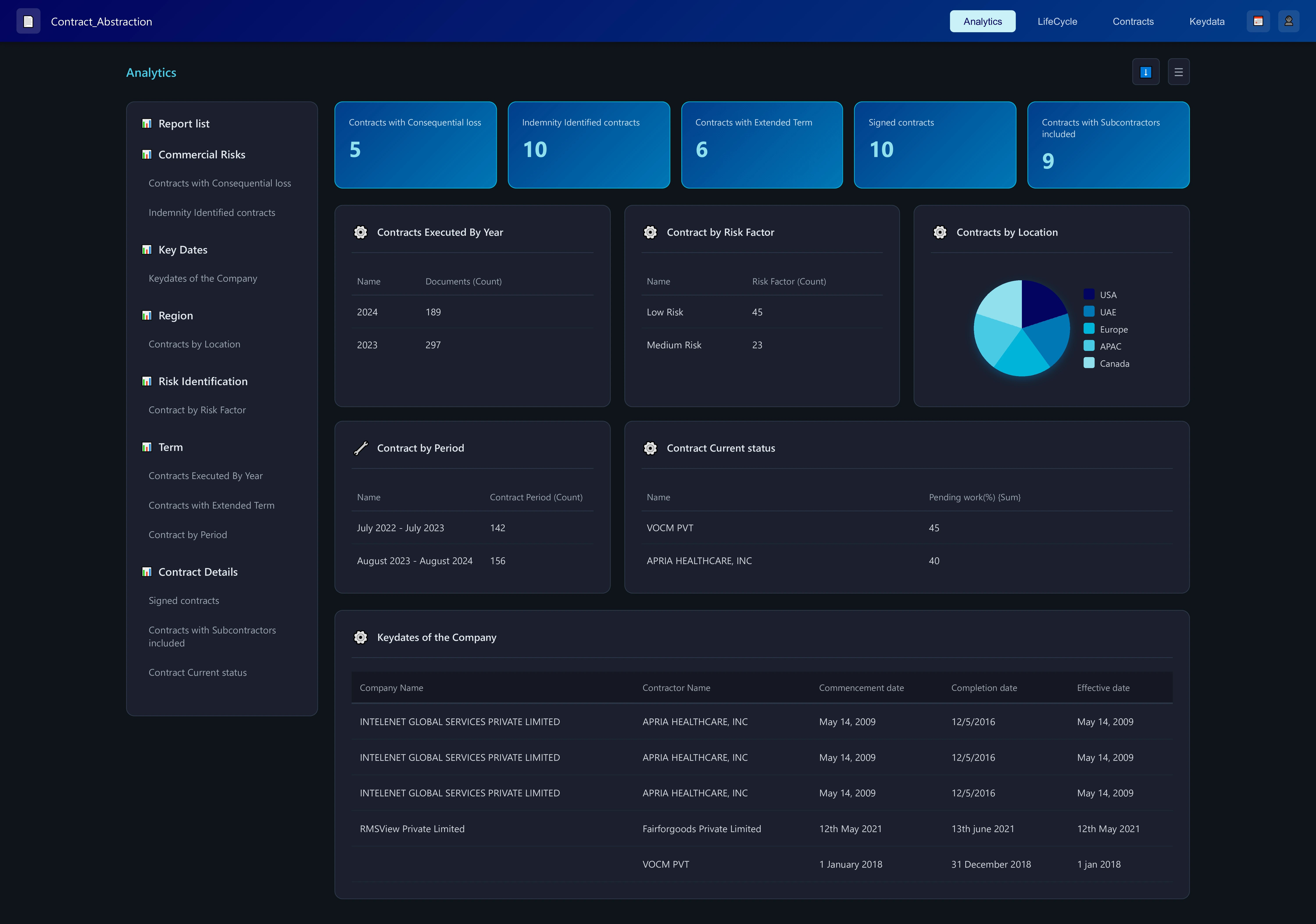
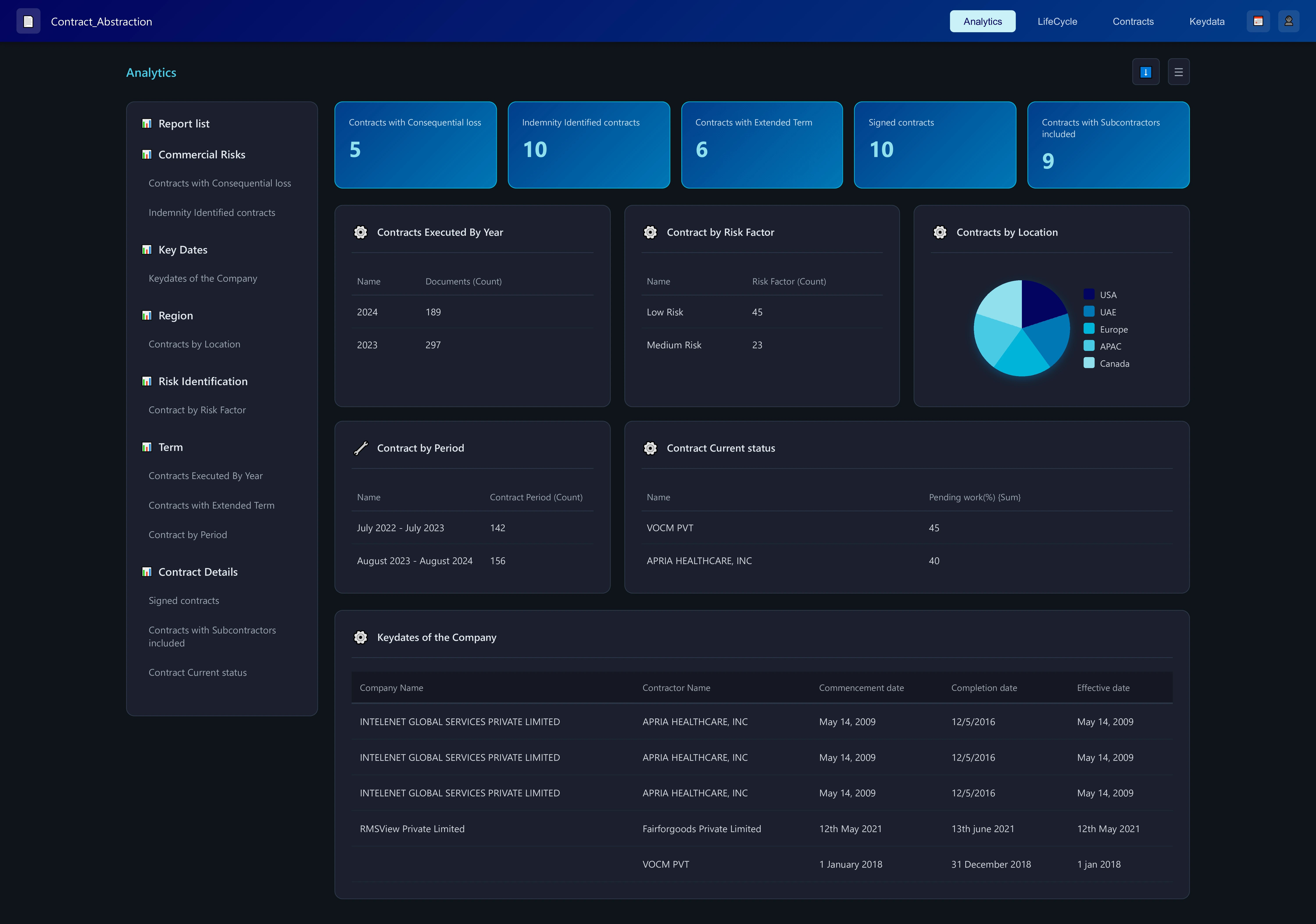
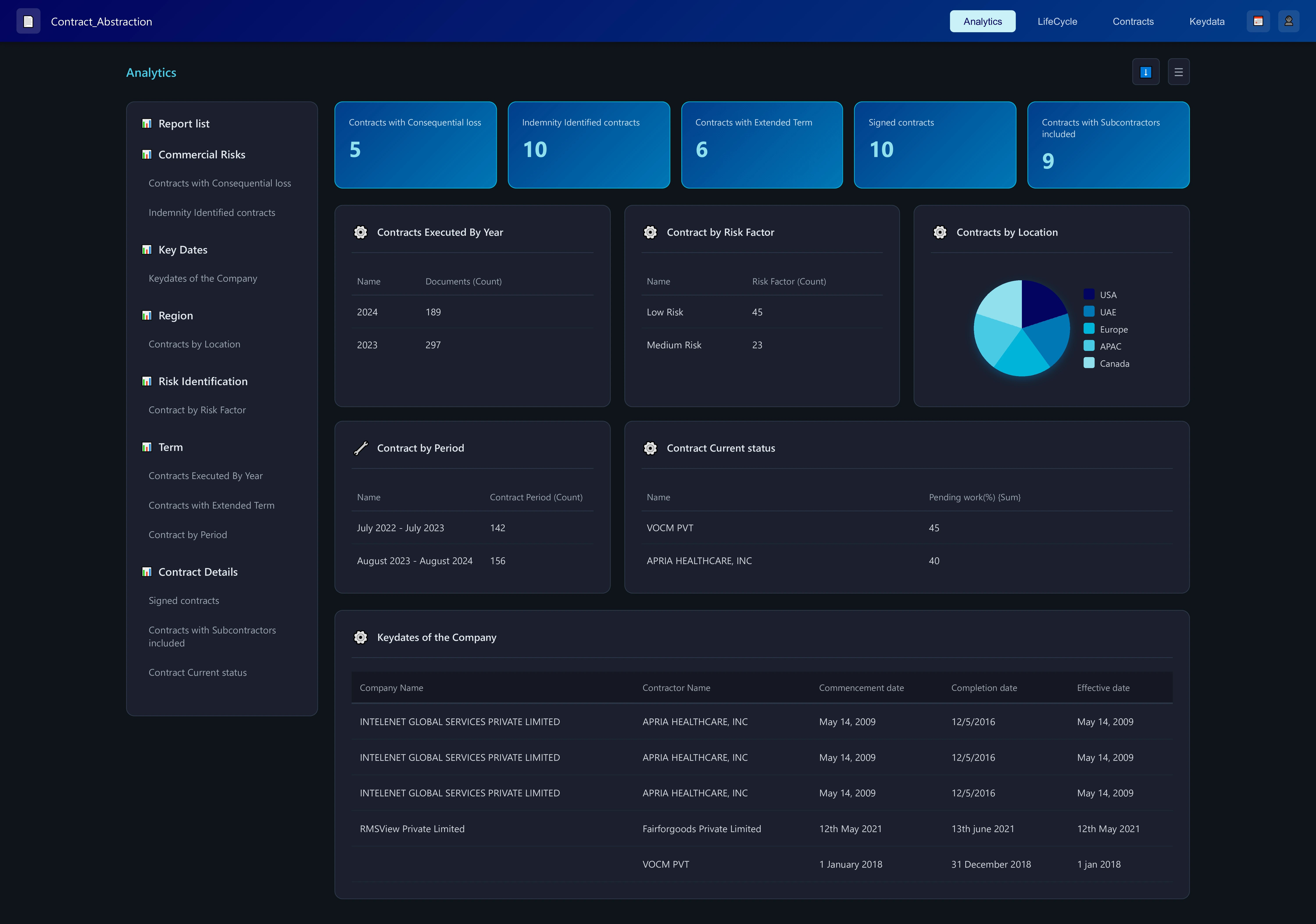
RCM Performance Suite is engineered for healthcare finance, billing ops, and revenue integrity teams. It consolidates patient encounters, claim forms, and medical records—regardless of format—and surfaces structured, decision-ready insights.
Anomalies and denial risks are flagged and ranked, with full traceability back to their origin in claims or clinical documentation. A rule engine applies your payer or policy logic, while performance dashboards visualize key metrics—turnaround times, denial trends, revenue leakage. As your team reviews and corrects, the system learns and refines future predictions.
The result: fewer denials, faster reimbursement cycles, and data you can audit, trust, and act on.
Clean Claims, Faster Payment – Optimized for Diagnostics
Shift from "post-denial recovery" to "pre-claim prevention." Achieve the collection rates required to sustain innovation in high-science markets.
reduction in Days Sales Outstanding (DSO)
decrease in administrative denial rate
success rate on automated prior authorizations
ROI on appeal recovery
See RCM Performance in Action
Watch how the suite transforms claims and health records into structured insights—driving measurable uplift in cycle efficiency and revenue integrity.
Automate Prior Auth
Submit clinical documentation to payer portals via bots to secure authorization numbers instantly, preventing front-end denials.
Generate Clinical Appeals
Automatically draft appeal letters for "medical necessity" denials, referencing specific patient history and payer policy guidelines.
Estimate Patient Cost
Calculate precise out-of-pocket expenses based on real-time deductible status to collect co-pays before the test is processed.
Predict Denial Risk
Score every claim before submission; if the risk is high, route it to a coding specialist to fix the error before it leaves the building.
Get the answers you need
Find clarity on our solutions, capabilities, and how we can support your business.
RCM is a critical, time-consuming and administratively heavy process that includes patient registration, insurance billing, verification with payors, coding the claim, payment and collection.
Errors and delays due to manual entry or checks across high volumes of documents leads to poor patient satisfaction; and delays in collections for the healthcare providers.
With a huge number of payors (over 900 in the US), health plans, validation checks required and regulations to comply with – health care providers outsource this critical back-office process to RCM service providers – who deploy large teams to handle this.
Pre-processing a claim filed needs to be done in a stipulated time frame – and this poses a challenge when done manually.
Automation of the RCM process enables RCM service providers turbocharge the entire process – handling claims in minutes with ~100 accuracy – they are thus able to increase the volume of records handled with the same time (nearly 3X)
Health care providers can also leverage automation to reduce manual efforts and streamline their RCM process.
The Botminds AI platform can handle all key financial statements in multiple formats, reporting/accounting standards and filing types across geographies - Balance sheets, Income statements, cash flows, Annual reports, SEC filings (10Q, 10K, 8K etc.); tax forms; Personal financial statements etc.
Botminds can handle any PDF documents (scanned or digital) - handwritten and/or printed. In addition, the Botminds AI platform can extract relevant payor, provider or other related unstructured data from web pages, if any.
In case of SaaS model, the data is highly secure with 2FA and role-based access controls in place. Botminds platform was built with high degree of data security in mind.The Botminds AI platform can also be deployed in a private cloud environment for our clients – this ensures that documents and data never leave the client’s environment.
Ready to Adapt, Grow, Optimize
or Disrupt With Us?
Book a 30-minute consultation to find the best starting point