Claims Resolution Platform
Resolve healthcare claim disputes faster—by surfacing inconsistencies, policy deviations, and high-risk items with full audit traceability.
Challenges
Claims operations break when manual adjudication processes cannot keep pace with rising volumes and complex coding standards. Intelligent automation is required to prevent backlog accumulation and leakage from improper payments.
Fragmented Clinical Data
Claims arrive via EDI, scanned HCFA/UB-04 forms, and faxed medical records. Disconnected data sources make cross-referencing clinical evidence with billing codes manually impossible.
High Denial Rates
Manual reviews of CPT and ICD-10 codes against policy guidelines are prone to error. Inconsistent application of rules leads to avoidable denials and provider abrasion.
Fraud and Waste Leakage
Detecting patterns of upcoding, unbundling, or duplicate billing requires analyzing historical data at scale. Human reviewers miss subtle fraud signals in individual claim files.
Slow Reimbursement Cycles
The lag time between claim receipt and final payment decision stretches weeks. Administrative delays impact cash flow for providers and member satisfaction scores.
What Defines Us
Redefining claims lifecycle management with clinical intelligence that turns raw medical documents into auto-adjudicated payment decisions.
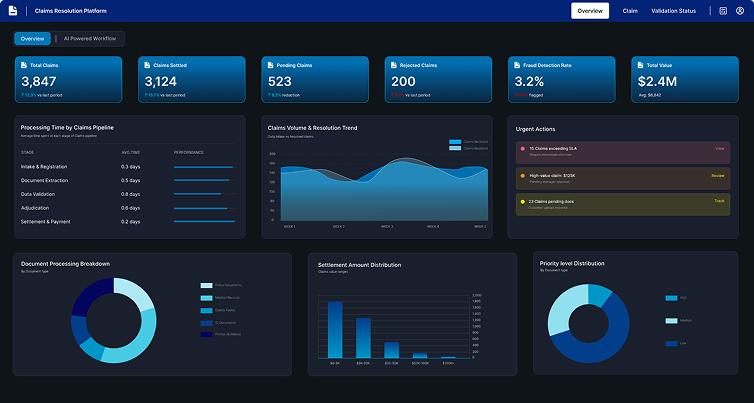
AI-Powered Claims Adjudication for Accuracy and Scale
Deploy intelligent agents to autonomously ingest and digitize complex claim packets, including structured EDI streams and unstructured medical attachments. The system identifies, extracts, and correlates member data, procedure codes, and diagnosis descriptions across thousands of claims simultaneously, regardless of the submission format.
Ensure payment integrity through automated validation workflows that cross-reference billed codes against payer policies and medical necessity guidelines. The platform handles exceptions by flagging high-cost or ambiguous claims for nurse review while auto-adjudicating routine submissions. Beyond processing, the solution delivers intelligence by detecting billing anomalies indicative of fraud or waste, stopping improper payments before they occur.
Touchless, Accurate Claims Processing – In Real Time
Move from manual review to automated decisioning. Achieve the Straight-Through Processing (STP) rates required to reduce administrative costs and improve provider relationships.
increase in auto-adjudication rates
reduction in processing cost per claim
coding accuracy
faster reimbursement cycle
See Resolution Intelligence in Action
Observe how the platform surfaces claim discrepancies, policy deviations, and resolution paths—turning dispute workloads into actionable, auditable insight.
Eliminate Manual Data Entry
Automatically capture data from paper claims and scanned attachments to feed adjudication engines instantly.
Stop Leakage Early
Detect and flag upcoding, unbundling, and duplicate submissions in real-time to prevent overpayment.
Scale Without Backlogs
Handle seasonal spikes in claim volume (e.g., end-of-year) without hiring temporary adjudication staff.
Ensure HIPAA Compliance
Maintain rigorous data security and audit trails for every claim decision, ensuring protection of PHI (Protected Health Information).
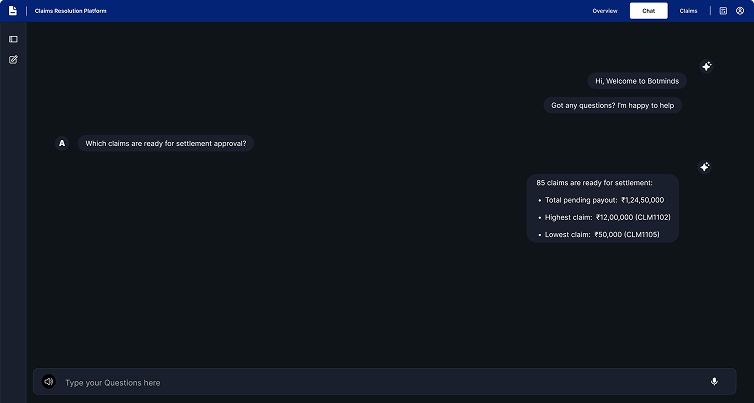

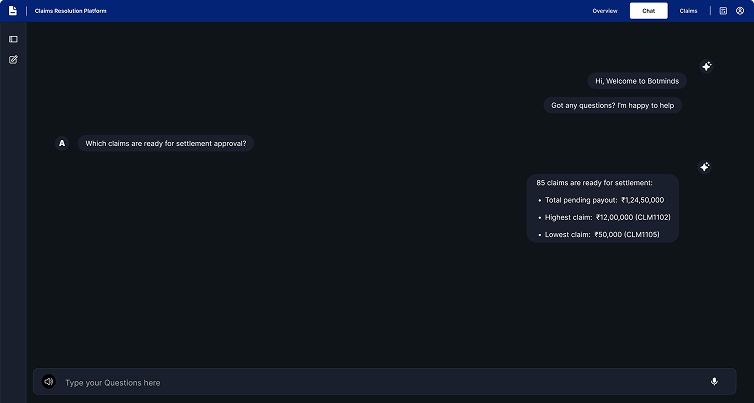
Get the answers you need
Find clarity on our solutions, capabilities, and how we can support your business.
Accounting standards differ by countries and regions as they have evolved based on the historical norms, legal and taxation procedures.
The US Generally Accepted Accounting Principles (US GAAP) is not followed across the world. The International Financial Reporting Standards (IFRS), currently followed by 120+ countries, was derived based on guidelines provided by the London-based International Accounting Standards Board (IASB) - to have an international accounting framework.
There were over 15+ IFRS and 20+ International Accounting Standards as of 2019. The IAS will replace IFRS when it finalized by IASB.
All of this makes it challenging to compare and analyse financial statements of companies with cross-border commerce; or those across geographies – since it is largely manually and is an error-prone, tedious job. An AI-powered financial spreading automation platform such as Botminds AI is designed to address this very challenge.
Restatements (and remediations) can be triggered due to wrongly applied complex accounting or taxation rules such as acquisitions, revenue recognition; errors in classifying cash flows; revisions in estimations (e.g. depreciation of assets); and gaps in internal controls. Adoption or changes in systems used such as ERP, Accounting software etc. - may also lead to need to remediation of financial processes and statements.
Botminds can handle any PDF documents (scanned or digital). In addition, the Botminds AI platform can extract unstructured data from financial tables or text on web pages, if any.
Your data is highly secure. Botminds platform was built with high degree of data security in mind. 2FA and role-based access controls are in place.
Ready to Adapt, Grow, Optimize
or Disrupt With Us?
Book a 30-minute consultation to find the best starting point